 When most people hear the diagnosis of sepsis, they think of one of two things: oh my god or…what the heck is that? However, when I see the diagnosis of sepsis, my mind turns to one thing which I call the sepsis umbrella. For the sepsis umbrella to make sense, let’s first define what sepsis is and why this particular disease is so baffling.
When most people hear the diagnosis of sepsis, they think of one of two things: oh my god or…what the heck is that? However, when I see the diagnosis of sepsis, my mind turns to one thing which I call the sepsis umbrella. For the sepsis umbrella to make sense, let’s first define what sepsis is and why this particular disease is so baffling.
Sepsis is often defined as an uncontrolled systemic immunological response to an infection through which progression can result in organ dysfunction and death. This is not the only definition of sepsis as, in 2016, sepsis was redefined as a “life threatening organ dysfunction caused by a dysregulated host response to infection”, aka Sepsis-3 (Singer, et al.). If this wasn’t already convoluted enough, it gets worse as there is an additional subsection of sepsis known as septic shock. Septic shock is a highly severe form of sepsis where “underlying circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than sepsis alone” (Shankar-Hari, et al.). This is a lot to unravel and there’s no better place to start then with the actual symptoms and progression of sepsis. 
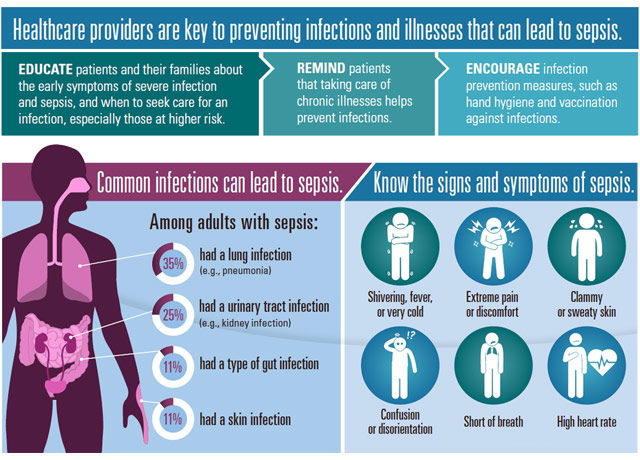
At this point you probably won’t be surprised when I tell you that, like its definition, the symptoms of sepsis are very non-specific. A patient with a mild case can appear almost asymptomatic while other sepsis patients can be at death’s door. So how is sepsis even diagnosed? Generally, a patient diagnosed with sepsis will have a pre-existing infection such as skin or wound infections, infections to a surgical site, or even viral infections. The initial infection must also present with symptoms that fall under the systemic inflammatory response syndrome (SIRS) or the multiorgan dysfunction syndrome (MODS) criteria to be qualified as sepsis.
The SIRS criteria consist of four key symptoms: fever, tachycardia (elevated heart rate), tachypnea (breathing fast), and leukocytosis (elevated white blood cell count). To have sepsis a patient must have an initial infection coupled with 2 of the SIRS symptoms. As the infection and uncontrolled immune response progresses past the SIRS criteria, the patient begins to experience a decline in peripheral vascular perfusion (decreased blood flow to peripheral tissues) and tissue hypoperfusion (decreased blood flow to the organs). At this point the patient is entering septic shock as their body continues its inflammatory response with decreased blood movement and increased organ dysfunction. If the patient is being treated at this time but continues to decline, then they have reached MODS criteria and are in critical state. Unfortunately, there is a 75% mortality rate after MODS is reached.
So why bring all of this up? While sepsis is a diagnosis on its own, it is not a disease that begins without an initiating infection. This is important because it can have massive effects on the way we study sepsis. Consider this: sepsis can stem from any form of infection including viral infections, fungal infections, and bacterial infections. Each of these infections have a different infectious process and they can result in sepsis at different rates, frequencies, and severities.
Furthermore, when do we classify an infection as being septic rather than a natural progression of the disease? For example, there are many symptom similarities between severe COVID-19 (progressed infection leading to decreased oxygen levels, tachycardic, fever, etc.) as sepsis, which could classify many COVID-19 patients as having sepsis. And yet, these patients are not classified as having sepsis. Additionally, a patient with cancer may produce laboratory results that correlate with sepsis but not actually be septic. How do you narrow this down to form one conclusive definition and treatment? Simply put, you can’t. Sepsis is, by its epidemiology and definition, an umbrella term.
This sepsis umbrella is detrimental for scientists studying sepsis. To counter this, I’d like to propose a new use of the sepsis umbrella. Instead of diagnosing sepsis at any progressed infection with uncontrolled immune response, we should shift to describing an infection as becoming septic rather than being sepsis. While this may seem like a simple change, it opens the door for researchers to specify what they are studying and to consider how individual pathogens are able to produce such drastic responses. Shifting our use of sepsis would also prevent infections, such as COVID -19, from being ruled out of this definition due to their prevalence or acute manifestations. Ultimately, getting rid of the sepsis umbrella isn’t the answer but we do need to learn how to close it. After all, opening an umbrella indoors is bad luck.
References:
Center of disease control: What is sepsis – https://www.cdc.gov/sepsis/what-is-sepsis.html
Gyawali, B., Ramakrishna, K., & Dhamoon, A. S. (2019). Sepsis: The evolution in definition, pathophysiology, and management. SAGE open medicine, 7, 2050312119835043. https://doi.org/10.1177/2050312119835043
Huang, M., Cai, S., & Su, J. (2019). The Pathogenesis of Sepsis and Potential Therapeutic Targets. International journal of molecular sciences, 20(21), 5376. https://doi.org/10.3390/ijms20215376
Koçak Tufan, Z., Kayaaslan, B., & Mer, M. (2021). COVID-19 and Sepsis. Turkish journal of medical sciences, 51(SI-1), 3301–3311. https://doi.org/10.3906/sag-2108-239
Mahapatra S, Heffner AC. Septic Shock. [Updated 2022 Jun 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430939/
Markwart, R., Saito, H., Harder, T., Tomczyk, S., Cassini, A., Fleischmann-Struzek, C., Reichert, F., Eckmanns, T., & Allegranzi, B. (2020). Epidemiology and burden of sepsis acquired in hospitals and intensive care units: a systematic review and meta-analysis. Intensive care medicine, 46(8), 1536–1551. https://doi.org/10.1007/s00134-020-06106-2
Shankar-Hari, M., Phillips, G. S., Levy, M. L., Seymour, C. W., Liu, V. X., Deutschman, C. S., Angus, D. C., Rubenfeld, G. D., Singer, M., & Sepsis Definitions Task Force (2016). Developing a New Definition and Assessing New Clinical Criteria for Septic Shock: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA, 315(8), 775–787. https://doi.org/10.1001/jama.2016.0289
Singer, M., Deutschman, C. S., Seymour, C. W., Shankar-Hari, M., Annane, D., Bauer, M., Bellomo, R., Bernard, G. R., Chiche, J. D., Coopersmith, C. M., Hotchkiss, R. S., Levy, M. M., Marshall, J. C., Martin, G. S., Opal, S. M., Rubenfeld, G. D., van der Poll, T., Vincent, J. L., & Angus, D. C. (2016). The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA, 315(8), 801–810. https://doi.org/10.1001/jama.2016.0287
World health organization: Sepsis – https://www.who.int/news-room/fact-sheets/detail/sepsis